Shavuot is a name derived from Hebrew that means ‘weeks’. It is a significant event for the Jews that arrives after fifty days of the Passover. From religious celebrations to enjoying delicious meals made from dairy products, there is so much people do during the Shavuot week! It is a beautiful harvest festival counted from the second-night post the Passover and lasts for seven weeks. The last day of the seven weeks is celebrated as Shavuot. During this time, the believers are firmly focused on commemorating the giving of the Torah and the marvellous revelation that happened at Mount Sinai in Egypt. It is a time for communal unity, prayers and enjoying the meals together made from the fresh harvest. Shavuot is all about enjoying the shared heritage and staying true to one’s faith.

Here’s everything you need to know about the Shavuot festival, its significance in ancient Israel, the giving of the Torah and the profound spiritual enlightenment that people aim for during these weeks.
Historical Background
In ancient Israel, Shavuot started as an agricultural festival which celebrated the end of the harvest season. It was closely connected with the crops’ agricultural cycle and represented the farmers’ agrarian lifestyle. The seven-week duration was more like a countdown from the Passover to the time of the first harvest in the spring season. The festivities used to end when the first fruit or Bikkurim of the wheat harvest was offered to the Lord at the temple of Jerusalem. It was a symbol of gratitude and recognition for what God offered to mankind. Not just wheat, but other harvests like barley, grapes, figs, olives, dates and even pomegranates were offered in the temple. These were known as the seven species or the seven kinds of foods grown in Israel.
Shavuot is one of the three pilgrimage festivals. The other two are Passover and Sukkot. The Israelites were commanded to appear in front of the Lord in Jerusalem along with their agricultural yield. This was not just some kind of religious obligation but also God’s way of saying that communal celebration and worship are two key things that can make the body and soul feel blissful.

The association of Shavuot with the giving of the Torah happened at a later point. However, it did add religious significance to the day which was otherwise believed to be only a harvest festival.
Though the Torah doesn’t specify that Shavuot is closely related to the giving at Mount Sinai, this was concluded based on chronological events. The Rabbinic tradition calculates that the day of Shavuot coincides with when God gave the Torah to the people at Mount Sinai.
The story begins when the Israelites were liberated from slavery in Egypt. This is the ‘Passover’. After leaving Egypt, they travelled for several days in the desert while facing harsh weather conditions and after seven weeks arrived at Mount Sinai with the help of Moses’ guidance.
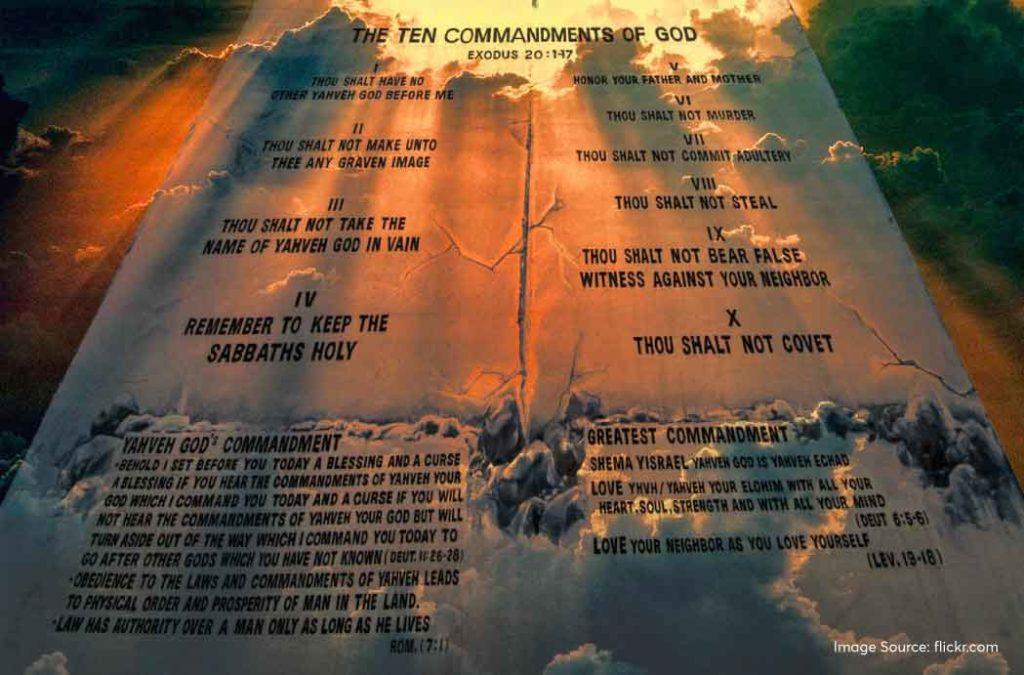
On the sixth day of the Sivan month, God appeared in front of the people and gave them the Torah. He also gave Moses the two stone tablets that contained the Ten Commandments. These commandments are the main foundation of the Torah and the Jewish law.
Religious Significance of Shavuot
The giving of the Torah is a direct connection between God and the people where he guides his disciples towards the right ethical lifestyle. The Israelites were very overwhelmed to see God Himself appear before them and requested Moses to be their intermediary so that he could learn more about the Torah and its explanations. He remained on Mount Sinai for forty days and nights to get the full Torah. He was given the written Torah which includes the first five books of the Hebrew Bible and also the oral Torah which includes the interpretations. These were later mentioned in the Talmud and other rabbinic texts.
The Ten Commandments lay down the rules of one’s responsibilities towards God and also fellow human beings. It established the covenant between people and the God. this is also referred to as the Mosaic Covenant and is a religious practice of paramount importance for Jews.
There is always something new to interpret from the Torah and the religious text never gets irrelevant. It is a means for lifelong learning and can be applied to contemporary situations if one can understand the interpretations better. The rabbinic authorities have always studied the Torah and tried to interpret the learning such that it can be used in the present Jewish laws to impart justice and peace. Shavuot is marked by dedicated Torah reading sessions precisely for this very reason. Children are especially encouraged to read the Torah so that they can know the right path of living and prove to be an asset to God and the community around them.
Traditions and customs
The days counted between the Passover and Shavuot are referred to as the ‘counting of Omer’. The word Omer meant the offerings of the first harvest that people took to the Lord in Jerusalem. Shavuot is now celebrated to commemorate the harvest and also to honour the Torah that was bestowed upon the believers.
The traditions and customs of Shavuot blend the historical significance of the harvest festival with the religious importance of the revelation at Mount Sinai. The things that people do on the day greatly reflect these two major events.
Counting of the Omer leading up to Shavuot
The Omer period connects the two major events in Jewish history. It starts from the day the Israelites were liberated from their harsh slavery to the day they were given the Torah at Mount Sinai. The period begins on the second night of Passover and ends on the eve of Shavuot. People indulge in prayers and spiritual enlightenment during the time span which lasts about 7 weeks or 49 days.

All night Torah study
Tikkun Leil Shavuot is one of the main traditions during the Shavuot festival. It refers to the all-night Torah reading sessions where people try to take away the life lessons taught by God Himself and implement them in their doings to have a better quality of life. It also represents the eagerness and happiness of people to accept the rules of God, something that their ancestors also did at Mount Sinai. The devotees gather at study halls, synagogues and at homes to read together all night. Along with the Torah, they also read other religious texts like the Talmud, the Book of Ruth, and other Jewish writings. They listen to religious commentaries as well.
Reading The Book of Ruth
The Book of Ruth tells the story of Ruth, a Moabite woman who married into the Jewish household of Naomi, her mother-in-law. The story is all about a woman’s loyalty to her mother-in-law, her kindness and her acceptance of Judaism.
Naomi is a widow. When her sons die, she urges her daughters-in-law to stay in her motherland and remarry. But this is where Ruth’s famous words come into the picture – “Where you go, I will go; where you stay, I will stay. Your people will be my people, and your God my God”.
She follows her mother-in-law to Bethlehem from Moab and indulges in agricultural activities for livelihood. This is how Shavuot started to be associated with the harvest season. Ruth eventually marries Boaz on Naomi’s persuasion and becomes the great-grandmother of King David.
Ruth’s life teaches people the importance of loyalty, kindness, empathy and the acceptance of the Jewish faith. People read her story on the holy night of Shavuot to appreciate the values that she showed.

Eating dairy food
Milk is an ingredient that has all the nutrition to sustain life. It is what a mother gives to her child to nurture him before he sets out to see the outer world. The Torah is compared with milk, a pure and pristine ingredient which nourishes a person. There is a Biblical reference in Song of Songs (4:11) that says “Milk and honey are under your tongue”, which tells that the Torah is as useful as the milk and as sweet as the honey.
This is why people make various dairy-based meals on Shavuot. Some of the famous dishes include cheesecakes, blintzes, Atayef – cheese-filled pastries, Kelsonnes – cheese-filled ravioli and cheese kreplach – dumplings. The Yemenite Jews do not have dairy products on Shavuot.
Decorating homes and synagogues with flowers and greenery
Shavuot is a harvest festival when the earth blooms to give its best offerings to mankind. Also, it is said when God was offering the Torah to Moses and the people, the entire Mount Sinai came to life with colourful flower blooms and swaying greenery. This is why the people decorate their houses and the synagogues with flowers and green plants to honour the harvest festival and the giving of the Torah.
It is fascinating to listen to the stories of the Jewish community, isn’t it? If you plan to meet Jewish people in India and get firsthand accounts of their religious practices, we suggest you pay a visit to Kerala and meet the Cochin Jews. While you are there, explore the breathtaking landscapes, and marvellous backwaters. You can also eat delicious local cuisines there.
Modern-Day Celebrations
In 2024, Shavuot will be celebrated from the evening of 11th June to 13th June.
The modern-day celebrations resemble the ones that people used to do way back in the olden days. The Jews decorate their houses with flowers and plants, dress in new clothes and set out to gather in communities or meet family members. Shavuot is the holiday season when people do not indulge in creative work and strictly dedicate their time to spirituality and religion.
The all-night Torah reading sessions are mandatory and people gather in religious places, houses, halls and synagogues to read together. They also try to make contemporary interpretations of the holy text. Many community halls, educational institutions and synagogues organise mass Torah study sessions. They also read the Book of Ruth on the night.
The festive meals are the fun part of Shavuot! The meals are cooked at home and shared with family, neighbours and people of the community. They gather in potlucks, share traditional recipes and enjoy the perfect holiday meals.
However, the Shavuot celebrations differ from place to place.

In Israel, schools, businesses and even government offices are closed on the day. There are several celebrations where people offer fresh harvest to God, spend time in agricultural fairs and also have kibbutz (a communal farm) celebrations. The celebrations happen only for a day.
In other parts of the world with Jewish population, the events may not be as grand as in Israel. Not all schools and businesses but the ones with Jewish roots are closed. They gather in religious activities, read the Torah together and spend quality time with family while eating dairy food. The celebrations may last for two days.
This change in the duration of the Shavuot festival is because of the ancient practices of their respective ancestors and the change in festival timings of the Jewish calendars from different regions.
FAQs
1 – When is Shavuot celebrated?
A – Shavuot is celebrated on the second night after the Passover and lasts for two days. According to the Jewish calendar, it can fall during the months of May and June. In 2024, the festival dates are from the evening of 11th June to 13th June.
2 – Why is Shavuot also called the Feast of Weeks?
A – Shavuot is called the feast of weeks because people wait for the first harvest for 7 weeks from the day of Passover to Shavuot. They count the days during this time. This is referred to as ‘counting of Omer’. Omer refers to the first harvest of the season.
3 – What are the main customs associated with Shavuot?
A – The main customs associated with Shavuot are all-night Torah study, offering the first harvest to God, eating dairy products, recital of prayers and reading the Book of Ruth.
Shavuot signifies the harvest season. It is a festival when people thank God for the first harvest, a way to show gratitude and thankfulness for what He bestows upon humankind. Also, it commemorates the day when God came to Earth and handed the Torah to people on Mount Sinai. The day is meant for spiritual reflection, peace and harmony among communities. This is when people read the Torah and embrace the ethical way of living.
Have you experienced the joy of the Shavuot festival before? Please let us know about your experience in the comments section below!